Medical Justice provides consultations to doctors facing medico-legal obstacles. We have solutions for doctor-patient conflicts, unwarranted demands for refunds, online defamation (patient review mischief), meritless litigation, and a gazillion other issues. We also provide counsel specific to COVID-19. If you are navigating a medico-legal obstacle, visit our booking page to schedule a consultation – or use the tool shared below.
“Can Medical Justice solve my problem?” Click here to review recent consultations…
all. Here’s a sample of typical recent consultation discussions…
- Former employee stole patient list. Now a competitor…
- Patient suing doctor in small claims court…
- Just received board complaint…
- Allegations of sexual harassment by employee…
- Patient filed police complaint doctor inappropriately touched her…
- DEA showed up to my office…
- Patient “extorting” me. “Pay me or I’ll slam you online.”
- My carrier wants me to settle. My case is fully defensible…
- My patient is demanding an unwarranted refund…
- How do I safely terminate doctor-patient relationship?
- How to avoid reporting to Data Bank…
- I want my day in court. But don’t want to risk my nest egg…
- Hospital wants to fire me…
- Sham peer review inappropriately limiting privileges…
- Can I safely use stem cells in my practice?
- Patient’s results are not what was expected…
- Just received request for medical records from an attorney…
- Just received notice of intent to sue…
- Just received summons for meritless case…
- Safely responding to negative online reviews…
We challenge you to supply us with a medico-legal obstacle we haven’t seen before. Know you are in good hands. Schedule your consultation below – or click here to visit our booking page.
When it comes to keeping secrets, physicians are often held to different standards than attorneys.
Tarasoff v. Regents of the University of California, the state Supreme Court held that mental health professionals have a duty to protect people who are threatened with bodily harm by their patient. In the original 1974 decision, the lower court ruled the doctor merely had a duty to warn. In the California Supreme Court decision, the stakes were elevated to duty to protect the intended victim. This duty can be performed by notifying the police, notifying the intended victim, or taking other reasonable steps to protect the threatened person.
What led to this result?
Prosenjit Poddar, from Bengal, India, entered University of California at Berkeley as a graduate student in 1967. In 1968, he met Tatiana Tarasoff at a folk dancing class. They started dating.
Tarasoff confided she was seeing other men. Poddar started stalking her. His mental health deteriorated. He became depressed. He neglected his studies and his health. He started speaking disjointly. People noticed he frequently wept.
Poddar occasionally met with Tarasoff. He secretly tape-recorded their conversations, trying to discover why she did not love him.
In 1969, Tarasoff left the country to travel.
Poddar’s mental state improved, and he entered therapy with Dr. Lawrence Moore, a psychologist with the student health service.
Poddar revealed to his psychologist that he intended to kill his ex-girlfriend. Dr. Moore wrote to campus police explaining that Poddar was suffering from acute and severe paranoid schizophrenia. He recommended that Poddar be civilly committed as a dangerous individual.
He was.
Poddar was detained but released as his mental state appeared improved. Moore’s supervisor ordered Poddar not be further detained.
Tarasoff knew nothing of this. She received no warning. None.
When Tarasoff returned to campus, Poddar befriended her brother. Really. He moved in with him.
On October 27, 1969, Poddar stabbed his ex-girlfriend, Tarasoff, killing her. He was convicted of second-degree murder. His conviction was overturned on the grounds the jury received inadequate instructions. He was released on condition he return to India. He was then deported “where he reportedly married a lawyer and led a normal life.”
Tarasoff’s family sued Dr. Moore and various university employees.
This case percolated to the California Supreme Court.
It concluded a mental health professional has a duty to a patient AND to individuals specifically threatened by a patient.
Justice Mathew O. Tobriner wrote the holding in the majority opinion. “We conclude that the public policy favoring protection of the confidential character of patient-psychotherapist communications must yield to the extent to which disclosure is essential to avert danger to others. The protective privilege ends where the public peril begins.”
The court was split.
Justice Mosk wrote a partial dissent, arguing that (1) the rule in future cases should be one of the actual subjective prediction of violence on the part of the psychiatrist, which occurred in this case, not one based on objective professional standards, because predictions are inherently unreliable; and (2) the psychiatrists notified the police, who were presumably in a better position to protect Tarasoff than she would be to protect herself.
Justice Clark dissented, quoting a law review article that stated, “…the very practice of psychiatry depends upon the reputation in the community that the psychiatrist will not tell.”
This duty to warn or protect is legislatively mandated in almost half the states. Common law also supports that duty in 10 more states. Eleven states permit a doctor to break confidentiality to warn (without mandating such a warning). Six states have no case law or statutes providing guidance.
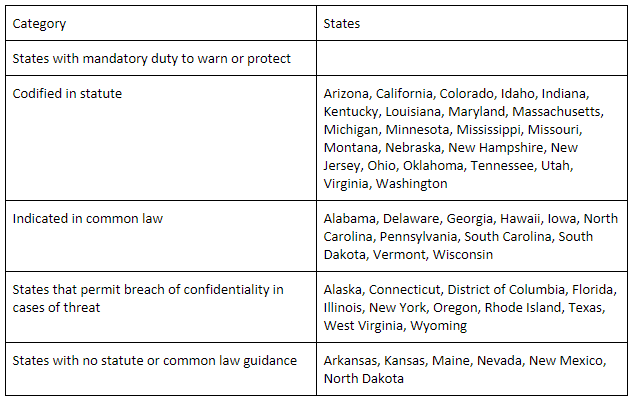
To make this even more confusing, states treat different health professionals differently.1
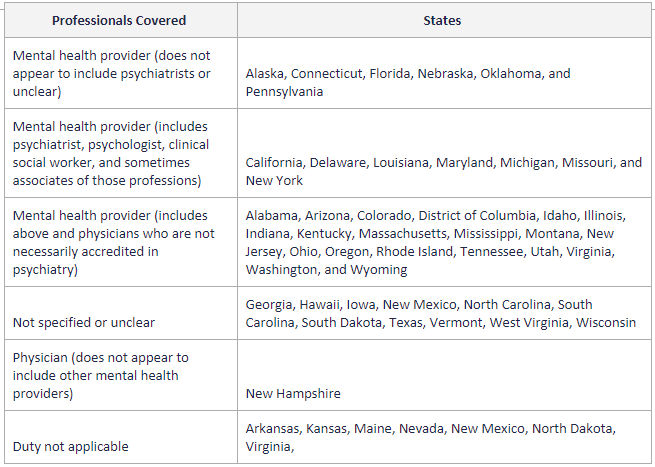
As one can see from the list, at least 20 states apparently extend the duty to physicians who are not necessarily credentialed in psychiatry, as long as the physician purports to offer mental health treatment.2
Please note, these state-by-state lists were published in 2014, and not may be up to date.
Surprisingly, predictions of courtroom doom and gloom for healthcare professionals have not materialized.
Soulier et al.3 in an analysis of 70 appellate cases from 1985 to 2006, found that 46 were decided in favor of the mental health professional, 6 were decided in favor of the plaintiff (although only 4 of these used Tarasoff statutes), and 17 were returned to trial courts for further litigation. Mental health professionals were exonerated on the following bases: no imminent threat was communicated to a therapist about an identifiable victim; the victim was already aware of the danger; or the therapist warned the victim, but the victim took actions that went against the warning.
Courts appeared to rule in favor of the victims only in marked cases of negligence by the mental health professional or institution: in Almonte,4 a psychiatrist/patient who was being seen by another psychiatrist admitted his sexual attraction to children but was recommended for a child psychiatry fellowship where he raped a child. In other cases, inpatient psychiatric treatment was terminated against medical advice or because the patient’s insurance coverage ran out.5
Tarasoff was a California court case.
Are California attorneys held to the same standard? If Prosenjit Poddar had been a client of an attorney, and Poddar confided he intended to kill Tatiana Tarasoff, then what? Does his attorney have to protect Ms. Tarasoff? Can he warn Ms. Tarasoff?
Under Rule 1.6 of the California Rules of Professional Conduct, Confidential Information of a Client6
A lawyer shall not reveal information protected from disclosure by Business and Professions Code section 6068, subdivision (e)(1) unless the client gives informed consent, or the disclosure is permitted by paragraph (b) of this rule.
A lawyer may, but is not required to, reveal information protected by Business and Professions Code section 6068, subdivision (e)(1) to the extent that the lawyer reasonably believes* the disclosure is necessary to prevent a criminal act that the lawyer reasonably believes* is likely to result in death of, or substantial* bodily harm to, an individual, as provided in paragraph
Before revealing information protected by Business and Professions Code section 6068, subdivision (e)(1) to prevent a criminal act as provided in paragraph (b), a lawyer shall, if reasonable* under the circumstances:
(1) make a good faith effort to persuade the client: (i) not to commit or to continue the criminal act; or (ii) to pursue a course of conduct that will prevent the threatened death or substantial* bodily harm; or do both (i) and (ii); and
(2) inform the client, at an appropriate time, of the lawyer’s ability or decision to reveal information protected by Business and Professions Code section 6068, subdivision (e)(1) as provided in paragraph (b).
In revealing information protected by Business and Professions Code section 6068, subdivision (e)(1) as provided in paragraph (b), the lawyer’s disclosure must be no more than is necessary to prevent the criminal act, given the information known* to the lawyer at the time of the disclosure.
So, a California lawyer may warn Tatiana Tarasoff, but he does not have to. And, if he does warn Ms. Tarasoff, he needs to first try to persuade his client to stand down. And then he has to tell his client he intends to warn.
From a practical perspective, I wonder how that plays out.
What do you think?
1 http://jaapl.org/content/42/4/469.long Rebecca Johnson, Govind Persad and Dominic Sisti. The Tarasoff Rule: The Implications of Interstate Variation and Gaps in Professional Training. Journal of the American Academy of Psychiatry and the Law Online December 2014, 42 (4) 469-477.
2 http://jaapl.org/content/42/4/469.long Rebecca Johnson, Govind Persad and Dominic Sisti. The Tarasoff Rule: The Implications of Interstate Variation and Gaps in Professional Training. Journal of the American Academy of Psychiatry and the Law Online December 2014, 42 (4) 469-477.
3 Soulier M, Maislen JD, Beck J. Status of the psychiatric duty to protect, circa 2006. J Am Acad Psychiatry Law 38:457–73, 2010.
4 Almonte v. New York Medical College, 851 F. Supp. 34 (D. Conn. 1994)
5 Soulier M, Maislen JD, Beck J. Status of the psychiatric duty to protect, circa 2006. J Am Acad Psychiatry Law 38:457–73, 2010.
6 https://www.calbar.ca.gov/Portals/0/documents/rules/Rule_1.6-Exec_Summary-Redline.pdf
Medical Justice provides consultations to doctors facing medico-legal obstacles. We have solutions for doctor-patient conflicts, unwarranted demands for refunds, online defamation (patient review mischief), meritless litigation, and a gazillion other issues. We also provide counsel specific to COVID-19. If you are navigating a medico-legal obstacle, visit our booking page to schedule a consultation – or use the tool shared below.
“Can Medical Justice solve my problem?” Click here to review recent consultations…
all. Here’s a sample of typical recent consultation discussions…
- Former employee stole patient list. Now a competitor…
- Patient suing doctor in small claims court…
- Just received board complaint…
- Allegations of sexual harassment by employee…
- Patient filed police complaint doctor inappropriately touched her…
- DEA showed up to my office…
- Patient “extorting” me. “Pay me or I’ll slam you online.”
- My carrier wants me to settle. My case is fully defensible…
- My patient is demanding an unwarranted refund…
- How do I safely terminate doctor-patient relationship?
- How to avoid reporting to Data Bank…
- I want my day in court. But don’t want to risk my nest egg…
- Hospital wants to fire me…
- Sham peer review inappropriately limiting privileges…
- Can I safely use stem cells in my practice?
- Patient’s results are not what was expected…
- Just received request for medical records from an attorney…
- Just received notice of intent to sue…
- Just received summons for meritless case…
- Safely responding to negative online reviews…
We challenge you to supply us with a medico-legal obstacle we haven’t seen before. Know you are in good hands. Schedule your consultation below – or click here to visit our booking page.
Learn how Medical Justice can protect you from medico-legal mayhem…
Take Advantage of Our Review Monitoring Service
With eMerit, we help you automate review collection and posting to improve your online reputation.
Consult with a Medico-Legal Expert
Medical Justice Founder and CEO, Jeff Segal, MD, JD and our expert team provide consultations to doctors in need of guidance.
Meet the Experts Driving Medical Justice
Our Executive Team walks with our member doctors until their medico-legal obstacles are resolved.
Jeffrey Segal, MD, JD
Chief Executive Officer and Founder
Dr. Jeffrey Segal, Chief Executive Officer and Founder of Medical Justice, is a board-certified neurosurgeon. Dr. Segal is a Fellow of the American College of Surgeons; the American College of Legal Medicine; and the American Association of Neurological Surgeons. He is also a member of the North American Spine Society. In the process of conceiving, funding, developing, and growing Medical Justice, Dr. Segal has established himself as one of the country’s leading authorities on medical malpractice issues, counterclaims, and internet-based assaults on reputation.
Dr. Segal was a practicing neurosurgeon for approximately ten years, during which time he also played an active role as a participant on various state-sanctioned medical review panels designed to decrease the incidence of meritless medical malpractice cases.
Dr. Segal holds a M.D. from Baylor College of Medicine, where he also completed a neurosurgical residency. Dr. Segal served as a Spinal Surgery Fellow at The University of South Florida Medical School. He is a member of Phi Beta Kappa as well as the AOA Medical Honor Society. Dr. Segal received his B.A. from the University of Texas and graduated with a J.D. from Concord Law School with highest honors.
In 2000, he co-founded and served as CEO of DarPharma, Inc, a biotechnology company in Chapel Hill, NC, focused on the discovery and development of first-of-class pharmaceuticals for neuropsychiatric disorders.
Dr. Segal is also a partner at Byrd Adatto, a national business and health care law firm. Byrd Adatto was selected as a Best Law Firm in the 2021 edition of the “Best Law Firms” list by U.S. News – Best Lawyers. With decades of combined experience in serving doctors, dentists, and other providers, Byrd Adatto has a national pedigree to address most legal issues that arise in the business and practice of medicine.




This is another one of those situations where the law is not clear, and we are expecting psychiatrists to be lawyers in the exam room. Professional organizations cannot even give clear guidance nationally because of the differences in state laws. The end result is chaos, because one would have to be a healthcare attorney specifically well versed in the nuances of these laws. But wait, there’s more — every case that gets decided by a different set of judges produces different rulings. Here’s another way that this could play out… blanket immunity of the physician for disclosing to law enforcement a threat made by a patient. This would be accompanied by a sign in the psychiatrists office that patients cannot disclose criminal acts to the psychiatrist because the psychiatrist may disclose it. This should also be part of the consent to treat form that the patient signs. Physicians need clear laws and rules to follow. They should not be trying to interpret case law and regulatory statutes, in the exam room. We need to stop regulating physicians to death and we need to shield them to the extent possible from ever changing laws. Physicians get tripped up because what is right today is wrong tomorrow. This is simply madness.
As to the issue of different laws for physicians and attorneys, what about equal protection under law. The law has to exist the same way for one group as it does for another. That is what justice is. If the standards of privacy and privileged information are different for different professions then you have conflict and chaos. We need less government intervention and rule making, more freedom, and more protection for physicians from liability.
Couple things…
There are several asterisks in the text, but no corresponding footnotes.
What was the decision against Moore? Against UC?
You differentiate between codified in statute and common law. I don’t know what that difference means.
Answer those and I might be able to form an intelligent opinion.
Hi Joe:
The six footnotes are included at the bottom of the blog post. University of California and Moore lost at appellate level. There, the judges made “new law” which is considered “common law.”
Alternatively, statutory law is passed by a legislature and signed into law by executive.
Both statutory and common law are part of our general legal system.