Medical Justice provides consultations to doctors facing medico-legal obstacles. We have solutions for doctor-patient conflicts, unwarranted demands for refunds, online defamation (patient review mischief), meritless litigation, and a gazillion other issues. We also provide counsel specific to COVID-19. If you are navigating a medico-legal obstacle, visit our booking page to schedule a consultation – or use the tool shared below.
“Can Medical Justice solve my problem?” Click here to review recent consultations…
all. Here’s a sample of typical recent consultation discussions…
- Former employee stole patient list. Now a competitor…
- Patient suing doctor in small claims court…
- Just received board complaint…
- Allegations of sexual harassment by employee…
- Patient filed police complaint doctor inappropriately touched her…
- DEA showed up to my office…
- Patient “extorting” me. “Pay me or I’ll slam you online.”
- My carrier wants me to settle. My case is fully defensible…
- My patient is demanding an unwarranted refund…
- How do I safely terminate doctor-patient relationship?
- How to avoid reporting to Data Bank…
- I want my day in court. But don’t want to risk my nest egg…
- Hospital wants to fire me…
- Sham peer review inappropriately limiting privileges…
- Can I safely use stem cells in my practice?
- Patient’s results are not what was expected…
- Just received request for medical records from an attorney…
- Just received notice of intent to sue…
- Just received summons for meritless case…
- Safely responding to negative online reviews…
We challenge you to supply us with a medico-legal obstacle we haven’t seen before. Know you are in good hands. Schedule your consultation below – or click here to visit our booking page.
An interesting thought experiment. Would you trade your leg for $20M?
The context. A med mal case with a jury verdict that delivered precisely that outcome.
The details.
The patient was a 43-year-old construction worker. So, he was young. At least I call that young.
In addition, he needed his leg to perform construction work. So, he was rendered unemployable in the primary domain he had mastered. More on that fact later.
He had a long history of lower back pain radiating down his left leg. He went to the ER on March 7, 2015 because his left foot pain felt different this time.
Two nurses documented his left foot was cool to the touch – and was turning purple.
Not a good sign. The physician assistant likely did not read the nursing notes and diagnosed the patient with worsening sciatica. And then discharged him.
The patient returned to the ER six days later with worsening pain – identified as 9/10. He was again seen by two nurses, one of whom had seen him on the first visit. So this nurse laid eyes on the patient twice. A nurse practitioner diagnosed the patient with…wait for it, yes, of course, sciatica. And sent the man home.
Four days later, this man was seen by his primary care physician. The pain continued unabated. An ultrasound showed deep venous thrombosis AND arterial thrombosis. He was quickly shuttled to the ER, where a vascular surgeon ordered a CT. The scan showed tissue necrosis. An above-the-knee amputation was performed the following day. According to the record, at the time the patient was evaluated by a vascular surgeon, the leg was not deemed salvageable.
The man’s Massachusetts medical malpractice lawyer argued to the jury that had an ultrasound been ordered during either of his client’s earlier emergency department visits, the DVT would have been diagnosed and treated, which would have avoided the amputation of his leg: “Honestly, the reason this happened was because the communication that happened in the emergency department between the nurses and providers was nonexistent.”
The Massachusetts medical malpractice jury awarded $10 million for the loss of his leg and an additional $10 million for the man’s pain and suffering. His lawyer, who had asked the jury to award the man $16 million, stated after the verdict: “I think it’s bittersweet. He understands that with a simple ultrasound [imaging test], he’d still have his leg.”
Interestingly, the patient was previously declared disabled because of a prior injury to his right leg.
An above the knee amputation is a bad outcome in anyone’s book. And I’m not minimizing the extent of the injury. But is it worth $20M? One driving factor of this jury verdict was the location of the trial. This took place in Massachusetts. Had this happened in a tort reform state, the verdict would have been capped at a lower amount. Here, $10M was for pain and suffering. In Texas, that number would have maxed out at $250k. Guess which state has high professional liability premiums?
For context, let’s examine the saga of a MIT biomedical engineer, Hugh Herr.
In 1982, Hugh Herr was in a tragic mountain climbing accident. He had frostbite. His doctors struggled for months to save his biological limbs. His legs were amputated and replaced with carbon and titanium composite prosthetics. He dreamed of climbing again.
Here, he is shown climbing 100ft above the ground – observe – no rope.
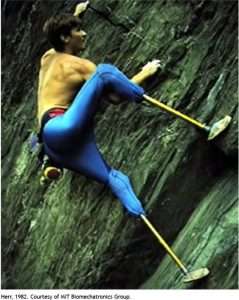
As an engineer, he designed new prosthetics where he could even adjust his height.
In his case, technology augmented his capabilities, beyond what human nature intended.
He was able to climb at a more advanced level than before being fitted with artificial limbs. He noted that there were no disabled people. Just disabled technologies.
Technology can improve upon biology.
In his talk, Dr. Herr noted that many in the audience were wearing eyeglasses. Such people would have been considered disabled – to some degree – at least vis a vis visual acuity. But, with eyeglasses, no longer.
Regarding his legs – he said he could not be considered disabled – “I climb mountains, for God’s sake.”
And, at 6:12 minutes in this video, take a look at US soldier with an above-the-knee amputation (fitted with a modern prosthetic) walking briskly on a treadmill at a pace that would be the envy of those in his neighborhood.
Herr concluded: “With my advanced prosthetic legs, I can stand, walk, run, and bounce. Ladies and gentlemen, welcome to the bionic age.”
So, would Hugh Herr have traded his biological limbs for $20M (or if you do the math properly, $40M)? I can’t say. Given what Hugh Herr was able to accomplish, would YOU trade a limb for $20M?
Medical Justice provides consultations to doctors facing medico-legal obstacles. We have solutions for doctor-patient conflicts, unwarranted demands for refunds, online defamation (patient review mischief), meritless litigation, and a gazillion other issues. We also provide counsel specific to COVID-19. If you are navigating a medico-legal obstacle, visit our booking page to schedule a consultation – or use the tool shared below.
“Can Medical Justice solve my problem?” Click here to review recent consultations…
all. Here’s a sample of typical recent consultation discussions…
- Former employee stole patient list. Now a competitor…
- Patient suing doctor in small claims court…
- Just received board complaint…
- Allegations of sexual harassment by employee…
- Patient filed police complaint doctor inappropriately touched her…
- DEA showed up to my office…
- Patient “extorting” me. “Pay me or I’ll slam you online.”
- My carrier wants me to settle. My case is fully defensible…
- My patient is demanding an unwarranted refund…
- How do I safely terminate doctor-patient relationship?
- How to avoid reporting to Data Bank…
- I want my day in court. But don’t want to risk my nest egg…
- Hospital wants to fire me…
- Sham peer review inappropriately limiting privileges…
- Can I safely use stem cells in my practice?
- Patient’s results are not what was expected…
- Just received request for medical records from an attorney…
- Just received notice of intent to sue…
- Just received summons for meritless case…
- Safely responding to negative online reviews…
We challenge you to supply us with a medico-legal obstacle we haven’t seen before. Know you are in good hands. Schedule your consultation below – or click here to visit our booking page.
Jeffrey Segal, MD, JD
Chief Executive Officer and Founder
Dr. Jeffrey Segal, Chief Executive Officer and Founder of Medical Justice, is a board-certified neurosurgeon. Dr. Segal is a Fellow of the American College of Surgeons; the American College of Legal Medicine; and the American Association of Neurological Surgeons. He is also a member of the North American Spine Society. In the process of conceiving, funding, developing, and growing Medical Justice, Dr. Segal has established himself as one of the country’s leading authorities on medical malpractice issues, counterclaims, and internet-based assaults on reputation.
Dr. Segal was a practicing neurosurgeon for approximately ten years, during which time he also played an active role as a participant on various state-sanctioned medical review panels designed to decrease the incidence of meritless medical malpractice cases.
Dr. Segal holds a M.D. from Baylor College of Medicine, where he also completed a neurosurgical residency. Dr. Segal served as a Spinal Surgery Fellow at The University of South Florida Medical School. He is a member of Phi Beta Kappa as well as the AOA Medical Honor Society. Dr. Segal received his B.A. from the University of Texas and graduated with a J.D. from Concord Law School with highest honors.
In 2000, he co-founded and served as CEO of DarPharma, Inc, a biotechnology company in Chapel Hill, NC, focused on the discovery and development of first-of-class pharmaceuticals for neuropsychiatric disorders.
Dr. Segal is also a partner at Byrd Adatto, a national business and health care law firm. Byrd Adatto was selected as a Best Law Firm in the 2023 edition of the “Best Law Firms” list by U.S. News – Best Lawyers. With decades of combined experience in serving doctors, dentists, and other providers, Byrd Adatto has a national pedigree to address most legal issues that arise in the business and practice of medicine.




I don’t recall which race it was–there may have been more than one–but at least one of the competitors had artificial legs. And won. Some of the other competitors complained that he had an unfair advantage.
My question to them: how would you like to have that same advantage?
Had a DPM been on call to examine this patient, even a second year student at DPM school knows how to palpate dorsalis pedis and posterior tibial pulses and would have immediately noticed a differential between one side and the other.
There are other signs, like dorsiflexion of the foot and squeezing the calf, which would have caused a significant response from the patient.
OK, I admit that DPM’s are highly sensitized to DVT and differences of pedal pulses. We know that at least in this case, such a consult was never even considered.
What does it cost to have a DPM on staff for an ER consult? Less than the settlement of this law suit, for sure.
Michael M. Rosenblatt, DPM
Let’s place the blame for the first case squarely where it belongs. Our medical system employees nurses, PAs and nurse practioners to examine patients. The physicians don’t even see the patients in the ER. Not even an eyeball. I know because I had an ER visit a couple of months ago, and I was never seen by the ER physician. I was seen by a nurse prac and then a nurse practitioner for the surgeon. I did not see the surgeon until I got to preop holding.
This method of treating patients is cheaper. But a nurse practitioner can never have the same training or experience as an ER physician, a surgeon, or an anesthesiologist.
Had a physician seen and examined the patient on the first visit and done a barebones physical exam, an ultrasound would have been ordered, the diagnosis confirmed, and treatment promptly started.
One second fault in this case, The PA did not see the nurses notes. Why? Because our EHR systems do more to hide relevant information rather than summarizing and presenting information in a way that is relevant and useful.
As I recall, the first Ebola case in Texas was missed because the nurses notes documenting travel outside the US to Africa were never seen by the ER physician. The patient died at home.
When I worked on EHR automatic record keeper prototypes, in the mid 1980s, we were worried, when a BP cuff and an arterial line on the same arm documented a zero BP when the BP cuff inflated. The other arm had the pulse ox and the IV.
In a conference of leading EHR experts at the Plaza Hotel in NY in 1985, I explained the above circumstances and stated that this false documentation on the part of the EHR was going to get us sued. The leading professors and chairman blew that off and said that we could just annotate the record. We stated that the flaw needed to be fixed to avoid false information getting into the record. Annotating the record, looks like trying to cover ones tracks in the event of a zero recorded pressure (even though false), to an attorney, if there is a bad outcome. Here we are 40 years later and there are now numerous instances, where the EHR hid information, or did not provide relevant information, creating other sorts of torts. The simple lack of full documentation that the EHR was conceived to correct in the 1980s pales by comparison to these types of cases.
We need to rethink having mid level practitioners and nurses doing triage and assessments. If we had physicians doing this, patients who needed to be seen for urgent matters would be treated better and faster. Those that needed PA or NP care could be directed to them. But it should be the physician doing the initial assessment.
When I was training younger residents, I always said to them… follow the TV show pronouncement 1 Adam 12 , 1 Adam 12 see the man. I told the residents not to depend upon a nurses assessment for a patient in the ICU at 3AM. Get up and go see the patient and assess them. I told them, you as a physician with your training will be better able to assess a patient and then decide if an issue is urgent or not.
My chief always trained us to look at the nurses notes which physicians rarely do, because they always had information that was important to know. We were trained to see if their assessment matched our own, and if not, to ask why not. Then as needed provide additional care and documentation.
These kinds of tragedies will just accelerate in our system as currently constituted.