Medical Justice provides consultations to doctors facing medico-legal obstacles. We have solutions for doctor-patient conflicts, unwarranted demands for refunds, online defamation (patient review mischief), meritless litigation, and a gazillion other issues. We also provide counsel specific to COVID-19. If you are navigating a medico-legal obstacle, visit our booking page to schedule a consultation – or use the tool shared below.
“Can Medical Justice solve my problem?” Click here to review recent consultations…
all. Here’s a sample of typical recent consultation discussions…
- Former employee stole patient list. Now a competitor…
- Patient suing doctor in small claims court…
- Just received board complaint…
- Allegations of sexual harassment by employee…
- Patient filed police complaint doctor inappropriately touched her…
- DEA showed up to my office…
- Patient “extorting” me. “Pay me or I’ll slam you online.”
- My carrier wants me to settle. My case is fully defensible…
- My patient is demanding an unwarranted refund…
- How do I safely terminate doctor-patient relationship?
- How to avoid reporting to Data Bank…
- I want my day in court. But don’t want to risk my nest egg…
- Hospital wants to fire me…
- Sham peer review inappropriately limiting privileges…
- Can I safely use stem cells in my practice?
- Patient’s results are not what was expected…
- Just received request for medical records from an attorney…
- Just received notice of intent to sue…
- Just received summons for meritless case…
- Safely responding to negative online reviews…
We challenge you to supply us with a medico-legal obstacle we haven’t seen before. Know you are in good hands. Schedule your consultation below – or click here to visit our booking page.
The National Practitioner Data Bank (NPDB) has over one million reports. Lots of data in this data bank.
Most of these reports relate to a professional liability carrier making payment on behalf of a doctor for an allegation of malpractice – either by settlement or judgment.
But those are not the only line items.
Disciplinary actions by state licensing entities are also reportable.
And professional review actions by hospitals or healthcare organizations restricting clinical privileges for more than 30 days are also reportable.
The Data Bank publishes a monthly newsletter with Q and A. Such newsletters usually begin with a vignette – “Is It Reportable?” Here’s a vignette from late 2021.
If my organization takes an action against a physician or other practitioner for not complying with our COVID-19 vaccination requirements, is it reportable?
It depends on both your organization type and the details of the action taken. If the action taken for not complying with an organization’s COVID-19 vaccination requirements meets the criteria for reporting of clinical privileges actions or reporting of other adjudicated actions or decisions (as laid out below and further explained in the Guidebook), then the action must be reported to the NPDB.
Hospitals and other health care entities must report adverse clinical privileges actions (infographic) that meet the reporting criteria of the NPDB. Clinical privileges include privileges, medical staff membership, and other circumstances (e.g., network participation and panel membership) in which a physician, dentist, or other health care practitioner is permitted to furnish medical care by a health care entity. Adverse clinical privileges actions that must be reported to the NPDB are actions that last for more than 30 days and are based on a physician’s or dentist’s professional competence or professional conduct that adversely affects, or could adversely affect, a patient’s health or welfare. Generally, the entity that takes the clinical privileges action determines whether the physician’s or dentist’s professional competence or professional conduct adversely affects, or could adversely affect, the health or welfare of a patient. (Reporting of physicians and dentists is mandatory. Other health care practitioners may be reported.) Administrative actions that are automatic in nature and are not the result of a professional review action are not reportable to the NPDB, because they are not considered clinical privileges actions.
Federal agencies, state law enforcement agencies, state Medicaid fraud control units, state agencies administering or supervising the administration of a state health care program, and health plans must report other adjudicated actions or decisions (infographic) against health care practitioners, providers, and suppliers (regardless of whether the action or decision is subject to a pending appeal). The term “other adjudicated actions or decisions” means: formal or official final actions taken against a health care practitioner, provider, or supplier that include the availability of a due process mechanism and that is based on acts or omissions that affect or could affect the payment, provision, or delivery of a health care item or service.
This language can be challenging to parse. I’ll dissect it in plain speak.
First, can a hospital suspend one’s clinical privileges for not receiving the COVID vaccine? There is federal law and state law on this topic. One law firm, Husch Blackwell, published an excellent post on state-by-state laws regarding mandatory vaccination as a condition of employment. The post was updated on February 23, 2022.
Under federal guidance, private employers can generally require employees to vaccinate against COVID-19, as long as they comply with federal laws that prohibit discrimination based on religion and disability. However, given the widespread availability of the COVID-19 vaccine, many states have proposed or enacted legislation prohibiting employers from mandating vaccinations or requiring proof of vaccination status. Similarly, many states have executive or administrative actions in effect that bar mandatory vaccination, either generally or as a condition of employment or receipt of services.
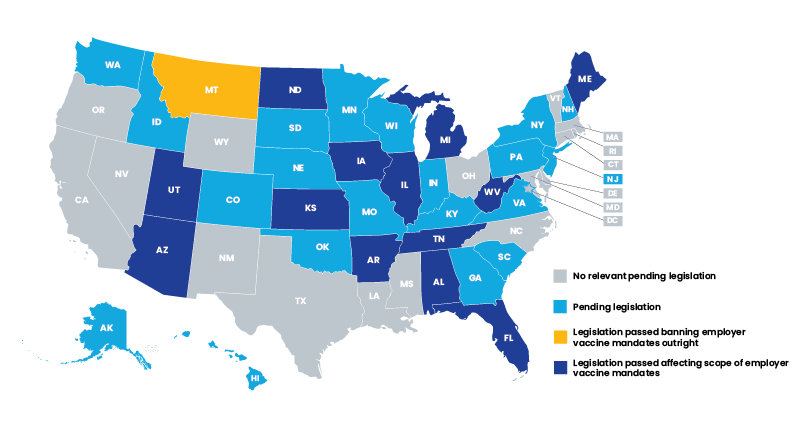
Different states come down on different sides of the issue.
New York City (note, as distinguished from New York state), for example, mandated order by Executive and Administrative Action that private employers with one or more employees (who perform in-person work or interact with the public) receive COVID -19 vaccination by December 27, 2021. This order extended beyond healthcare organizations. And it allowed for reasonable accommodations to be made for documented medical conditions or religious reasons.
In contrast, Texas mandated an order by Executive and Administrative Action that prohibited entities from requiring a COVID-19 vaccination for employees or consumers who object because of personal conscience, religious or medical reasons. The fine for violating that order was $1,000.
Now, back to the Data Bank.
If you work in a state that, under law, can mandate you take a COVID-19 vaccine as a condition of privilege, and you do not qualify for an applicable exception, is it reportable to the Data Bank?
It will depend upon how any action on clinical privileges is characterized.
If the action is a restriction of clinical privileges for more than 30 days and is based on a physician’s professional competence or professional conduct that adversely affects, or could adversely affect, a patient’s health or welfare, then the entity MUST report. Note that the Data Bank does not adjudicate whether or not the suspension could adversely affect patient welfare. This is determined at the hospital level.
Meaning, if the hospital concludes you’re not getting a COVID vaccine was the reason for suspension of privileges lasting more than 30 days and the hospital believed that such refusal could impact patient care, odds are high it would be reportable to the NPDB.
This conclusion is troubling for several reasons.
It means that where you practice is one determinant of whether the exact same actions would lead to a hospital reporting you – or not – to the NPDB. In a Kafkaesque twist, imagine you have licenses in multiple states. One state prohibits mandatory vaccinations. The other state allows for mandatory vaccinations. Now imagine your privileges are restricted by a hospital in the latter state. This gets reported to the Data Bank. Now the state that prohibits mandatory COVID-19 vaccinations learns of the discipline. From the Data Bank. Can it mete out reciprocal discipline? Yep. Will it? Dunno.
Next, current evidence suggests that the vaccine is mostly beneficial for preventing serious disease in the person receiving the vaccine. There are no compelling data to support the hypothesis that the vaccine prevents infection itself or decreases transmissibility. In other words, it’s unclear whether a physician refusing vaccination impacts patient safety. Yes, if a doctor has COVID (a different question entirely), his patients are at increased risk for getting COVID. So, doctors with active COVID should not knowingly expose their patients to their infection. But the presence or absence of COVID vaccination (as an isolated data point) does not move the needle on whether that doctor’s patients are at increased risk for infection.
Given the reputational damage that flows from a NPDB report, will hospitals actually characterize refusal to vaccinate as an adverse clinical privilege action that is reportable? Hospitals likely have some discretion in the characterization. And to avoid litigation, many might just consider it analogous to an administrative action such as failure to take some minimal number of CME hours each year.
Nonetheless, it’s difficult to remain sanguine about a hospital’s good intentions. If a hospital sees an opening to remove a “noisy” physician from its staff and keep him/her from moving operations to a competing facility, there’s no easier way to do it than submitting a timely Dara Bank report.
What do you think?
Medical Justice provides consultations to doctors facing medico-legal obstacles. We have solutions for doctor-patient conflicts, unwarranted demands for refunds, online defamation (patient review mischief), meritless litigation, and a gazillion other issues. We also provide counsel specific to COVID-19. If you are navigating a medico-legal obstacle, visit our booking page to schedule a consultation – or use the tool shared below.
“Can Medical Justice solve my problem?” Click here to review recent consultations…
all. Here’s a sample of typical recent consultation discussions…
- Former employee stole patient list. Now a competitor…
- Patient suing doctor in small claims court…
- Just received board complaint…
- Allegations of sexual harassment by employee…
- Patient filed police complaint doctor inappropriately touched her…
- DEA showed up to my office…
- Patient “extorting” me. “Pay me or I’ll slam you online.”
- My carrier wants me to settle. My case is fully defensible…
- My patient is demanding an unwarranted refund…
- How do I safely terminate doctor-patient relationship?
- How to avoid reporting to Data Bank…
- I want my day in court. But don’t want to risk my nest egg…
- Hospital wants to fire me…
- Sham peer review inappropriately limiting privileges…
- Can I safely use stem cells in my practice?
- Patient’s results are not what was expected…
- Just received request for medical records from an attorney…
- Just received notice of intent to sue…
- Just received summons for meritless case…
- Safely responding to negative online reviews…
We challenge you to supply us with a medico-legal obstacle we haven’t seen before. Know you are in good hands. Schedule your consultation below – or click here to visit our booking page.
Jeffrey Segal, MD, JD
Chief Executive Officer and Founder
Dr. Jeffrey Segal, Chief Executive Officer and Founder of Medical Justice, is a board-certified neurosurgeon. Dr. Segal is a Fellow of the American College of Surgeons; the American College of Legal Medicine; and the American Association of Neurological Surgeons. He is also a member of the North American Spine Society. In the process of conceiving, funding, developing, and growing Medical Justice, Dr. Segal has established himself as one of the country’s leading authorities on medical malpractice issues, counterclaims, and internet-based assaults on reputation.
Dr. Segal was a practicing neurosurgeon for approximately ten years, during which time he also played an active role as a participant on various state-sanctioned medical review panels designed to decrease the incidence of meritless medical malpractice cases.
Dr. Segal holds a M.D. from Baylor College of Medicine, where he also completed a neurosurgical residency. Dr. Segal served as a Spinal Surgery Fellow at The University of South Florida Medical School. He is a member of Phi Beta Kappa as well as the AOA Medical Honor Society. Dr. Segal received his B.A. from the University of Texas and graduated with a J.D. from Concord Law School with highest honors.
In 2000, he co-founded and served as CEO of DarPharma, Inc, a biotechnology company in Chapel Hill, NC, focused on the discovery and development of first-of-class pharmaceuticals for neuropsychiatric disorders.
Dr. Segal is also a partner at Byrd Adatto, a national business and health care law firm. Byrd Adatto was selected as a Best Law Firm in the 2021 edition of the “Best Law Firms” list by U.S. News – Best Lawyers. With decades of combined experience in serving doctors, dentists, and other providers, Byrd Adatto has a national pedigree to address most legal issues that arise in the business and practice of medicine.




