We recently blogged about a healthcare worker who was on the receiving end of a needlestick injury. The source patient agreed to be tested for HIV and hepatitis B and C. While the initial HIV test was positive, repeat testing was negative. Great news. The healthcare worker had been placed on post-exposure prophylaxis and it was discontinued once the all-clear signal was received.
Most patients are cooperative and will give affirmative consent to test their blood.
What happens if the patients refuses consent? Is the healthcare worker out of luck? Do they just need to assume the patient may be HIV positive and take post-exposure prophylaxis if clinically indicated (assuming the benefit of medication outweighs the risk).
Well, actually the healthcare worker has options. In a 2012 article, Unconsented HIV Testing in Cases of Occupational Exposure: Ethics, Law, and Policy, the authors noted that 36 states (see 2012 list from that article below) have laws that allow unconsented HIV testing of source patients in select cases of occupational exposure when such exposure occurs to healthcare workers in hospital setting. These laws vary by state. And the list is likely different today than it was in 2012.
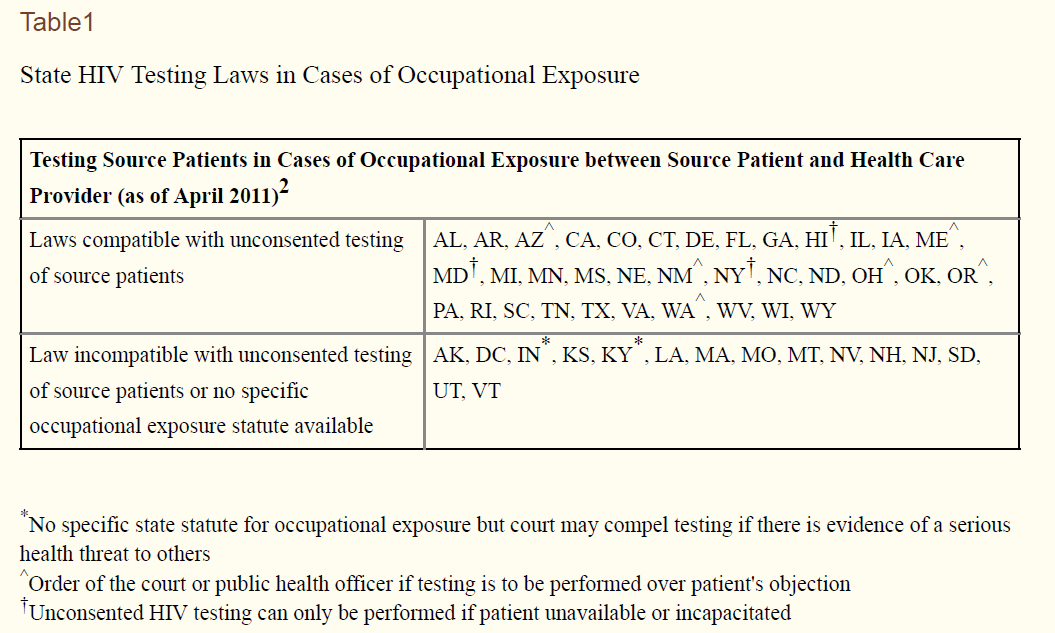
As of 2012, Arizona, Maine, New Mexico, and Oregon required a court order for all instances of unconsented HIV testing for occupational exposure. Most other states only required court order if blood specimen was not available for testing (the court order mainly being used to obtain the actual blood specimen itself).
Hawaii, Maryland, and New York permitted unconsented HIV testing in cases of occupational exposure only is source patients were unable to consent because they were absent, deceased, comatose, or lacked capacity to consent.
California, Rhode Island, and South Carolina permitted unconsented HIV testing on patients with full capacity even when they refuse voluntary testing.
In contrast, the federal government (overseeing care of VA patients) requires a patient’s verbal consent.
Q: If a source patient refuses testing, can I just test them anyway?
No. Federal law requires that VA patients give “full and informed consent” for any tests, and allows them the right to refuse any test or procedure. (August 2009)
Q: Other hospitals in my area do not require source patient consent for HIV testing during an occupational exposure. Why does VA?
As a part of the Federal Government, VA is subject to Federal laws, which may differ from State laws that govern the actions of other health care providers. In VA, all HIV testing of patients done for the purpose of establishing a diagnosis requires verbal informed consent of the veteran patient. (August 2009)
What is a patient refuses? One blogger who writes about North Carolina healthcare law gave practical information about how this can be addressed in North Carolina.
What if a known source person refuses to be tested?
The rules state that a source person may be tested with or without consent, so long as the test can be done with safety to the source person and the health care provider. In practice, providers should proceed with care if a source person refuses. A provider may try to persuade a source person to have the test, but should not restrain the person and force it. Instead, a source person who refuses testing should be reported to the local health director, who has legal authority to obtain information from other sources. The health director also has authority to enforce the communicable disease rules by instituting an action for injunctive relief in superior court (G.S. 130A-18) or seeking a misdemeanor charge against a person who refuses to comply with the rules (G.S. 130A-25; 130A-144(f)).
The take home point is that in many states there are options to identify whether or not a source patient is HIV positive in cases involving occupational exposure to a healthcare worker. This can help with guidance in use and timing of potential post-exposure prophylaxis. But, caution is in order. Every state is different. And the laws change over time. If you are stuck with such a needle, consider reaching out to the CDC (for medical guidance) and your local health department (for legal options) to come up with a plan for next steps.
What do you think? Let us know in the comments below.
Medical Justice provides consultations to doctors facing medico-legal obstacles. We have solutions for doctor-patient conflicts, unwarranted demands for refunds, online defamation (patient review mischief), meritless litigation, and a gazillion other issues. We also provide counsel specific to COVID-19. If you are navigating a medico-legal obstacle, visit our booking page to schedule a consultation – or use the tool shared below.
“Can Medical Justice solve my problem?” Click here to review recent consultations…
all. Here’s a sample of typical recent consultation discussions…
- Former employee stole patient list. Now a competitor…
- Patient suing doctor in small claims court…
- Just received board complaint…
- Allegations of sexual harassment by employee…
- Patient filed police complaint doctor inappropriately touched her…
- DEA showed up to my office…
- Patient “extorting” me. “Pay me or I’ll slam you online.”
- My carrier wants me to settle. My case is fully defensible…
- My patient is demanding an unwarranted refund…
- How do I safely terminate doctor-patient relationship?
- How to avoid reporting to Data Bank…
- I want my day in court. But don’t want to risk my nest egg…
- Hospital wants to fire me…
- Sham peer review inappropriately limiting privileges…
- Can I safely use stem cells in my practice?
- Patient’s results are not what was expected…
- Just received request for medical records from an attorney…
- Just received notice of intent to sue…
- Just received summons for meritless case…
- Safely responding to negative online reviews…
We challenge you to supply us with a medico-legal obstacle we haven’t seen before. Know you are in good hands. Schedule your consultation below – or click here to visit our booking page.





In the old days of communicable sexually transmitted diseases contact tracing and testing was a given. It was only when HIV came along and became a political disease. Since it primarily affected one group normal public health methods were abandoned. This is unfortunate.
Now the healthcare worker has to bear the burden for this legacy.
The counter point to this was the patient brought to an ER who was tested against their will by a police demand, ( I think it was for drugs) and the hospital personnel complied.
So there is a conflict between people’s rights and public safety. This is not going to be solved in the near future. There will likely be more litigation enacted, and more rules enforced to protect individual rights over the rights of the public.
In April 1993 I was working as an intern at Parkland Memorial Hospital in Dallas TX on the Neurosurgery service. I was changing a central line in the ICU post call (no work hour restrictions then) and had been up for over 24 hrs straight. I had a needle stick with a 22 gauge needle that I had used to localize the right IJ. I turned it in as a needle stick and I had my blood drawn and the family consented to testing the patient. One week later I was called by employee health that I had to come immediately to see them. It was then I was told that the patient was HIV positive and hep C positive. You can imagine my shock. Back then Parkland had a whole floor of patients with AIDS who were dying of terrible opportunistic infections. It was a death sentence if I converted. I was ushered down to the ER and was started on AZT 5 times a day and sent back to work. My wife was devastated. After 10 days I was so ill from the AZT that I could not work. It was either withdraw on a leave of absence or stop the AZT. I decided to stop the AZT given the very low chance of conversion and no proven efficacy of even taking AZT esp after one weeks time had passed. For one year I went every 3 months to check my HIV status. Fortunately, I never converted. That was a year of hell for me and my wife. What would have made it worse really was not knowing his HIV status. I never contracted hep C either. I still work some at my local va and the va policy is crazy wrong. Fortunately most patients agree to be tested now as there is at least treatment which can control the disease progression and it is not the death sentence that it once was. The previous comment is correct HIV needs to be treated like the sexually transmitted disease it is.
Readers of Medical Justice may not know that the State of California recently changed the law of a person KNOWINGLY subjecting another person by sexual contact to HIV AIDS. This has been changed from a felony to a misdemeanor.
The “idea” was to “reduce” the “stigma” of people with AIDS. Nowhere apparently was there a consideration of the drastic affect this diagnosis would have on the new recipient. Modern liberal press believes medical science has “cured” HIV AIDS. Or that it is no more serious than a bad cold.
Apparently California still allows “unconsented” HIV testing to occur. In the absence of consent, however, these extra steps are required:
“Instead of required written consent, H&S Code Section 120990(a) requires medical care providers to do the following before they order an HIV test:
1) Inform the patient that an HIV test is planned;
2) Provide information about the HIV test;
3) Inform the patient that there are numerous treatment options available for a patient who tests positive for HIV and that a person who tests negative for HIV should continue to be routinely tested;
4) Advise the patient that he or she has the right to decline the HIV test; and
5) If the patient declines the HIV test, document that fact in the patient’s medical file.”
The one thing obvious in the article is that the law is a hodgepodge or crazy quilt throughout the US. .
The only thing you can do as a healthcare provider is to LOOK UP the law in your state and be aware of it.
I was a surgical residency director many years ago. As a director, it is required that you have knowledge of the law in your state, since it is more than likely that if there is a resident exposure, they will contact YOU first.
Given a bent toward liberal political leanings occurring in some “target states” it may be more and more likely that medical personnel, rather than being assisted during their time of exposure, will be considered “disposable.”
Representative Pete Stark did all he could to criminalize doctors during his lengthy Congressional tenure.. I would not project any expectations for improvement for those exposed to infectious disease through no fault of their own. The authors of the previous posts are correct.
When it comes to politicization of communicable diseases, healthcare providers are at the bottom.
Michael M. Rosenblatt, DPM
The only time I took HIV prophylaxis (Truvada and Isentress) was after a needle stick from a known HIV patient. I was adjusting the needle while suturing and felt a tiny prick. After the procedure, I removed my gloves, squeezed my index finger and saw a drop of blood (Sleeping Beauty Princess Aurora moment). The price tag for a 6-week supply was several thousand dollars, and luckily, my insurance picked up the tab for the majority of the bill after getting ID “approval”. These drugs sucked the life out of me, and I have empathy for anyone who requires these meds ad infinitum for HIV-disease. Thankfully, I had a happy ending and did not fall into a deep sleep.
Do surgeons begin HIV prophylaxis after a needle stick if the patient denies HIV, and has no risk factors? If so, why not take Harvoni as well? Thank you.
If the HIV status is unknown as in needle cannot be traced to a specific patient e.g., needle left in bedding, or patient refuses to have HIV test done then prophylaxis is offered to you and ideally started within 4 hrs of exposure. Don’t know about Harvoni prophylaxis but in 1993 was not an option.
Two more cents – Is there a single case of HIV-disease transmitted to a surgeon after a lumen-free needle stick?
Is it Kosher to order HIV, and HepC titers on all patients BEFORE undergoing elective surgery, and refuse to perform surgery if the patient refuses?