In February, we published two articles related to patient reviews. One piece was published online. The second was made available for download. Both remain available, and we encourage our readers to study them. Considering the overwhelmingly positive reception both pieces received, we decided to return to the topic and discuss five more golden rules physicians should follow when responding to online reviews. Summarized, the questions this piece will answer are…
+ How should physicians thank patients for online reviews?
+ How should doctors respond to mixed reviews?
+ How should doctors respond to reviews that lack detail?
+ How should doctors deal with fake reviews posted by non-patients?
+ How should doctors deal with “review vigilantes?”
Without further ado – let’s begin…
Some doctors are in the habit of responding to positive patient reviews. If you are one of them, we understand the impulse. That said – we implore you to break the habit.
When a patient publishes a glowing review, it is tempting to interact with them. You may feel compelled to thank them. This is a natural response – most of us have been conditioned since childhood to thank those who take an action that benefits us.
We urge you to resist this urge.
Thanking the patient increases the likelihood you will betray his privacy. Even something as benign as
“You were a wonderful patient, Bill. You make my job easier.”
can be construed as a HIPAA violation. The reason is simple: Acknowledging the author’s status as your patient violates his privacy. The fact that the patient has just shared his experience online does not matter. If the patient wants to share that experience online, he has the freedom to do so. His doctor does not without the patient’s explicit (and signed) authorization.
Doctors know fines accompany HIPAA violations. Fewer know the exact costs associated with these fines. The graphic below will shed some light. Even “light” violations incur a stiff penalty.
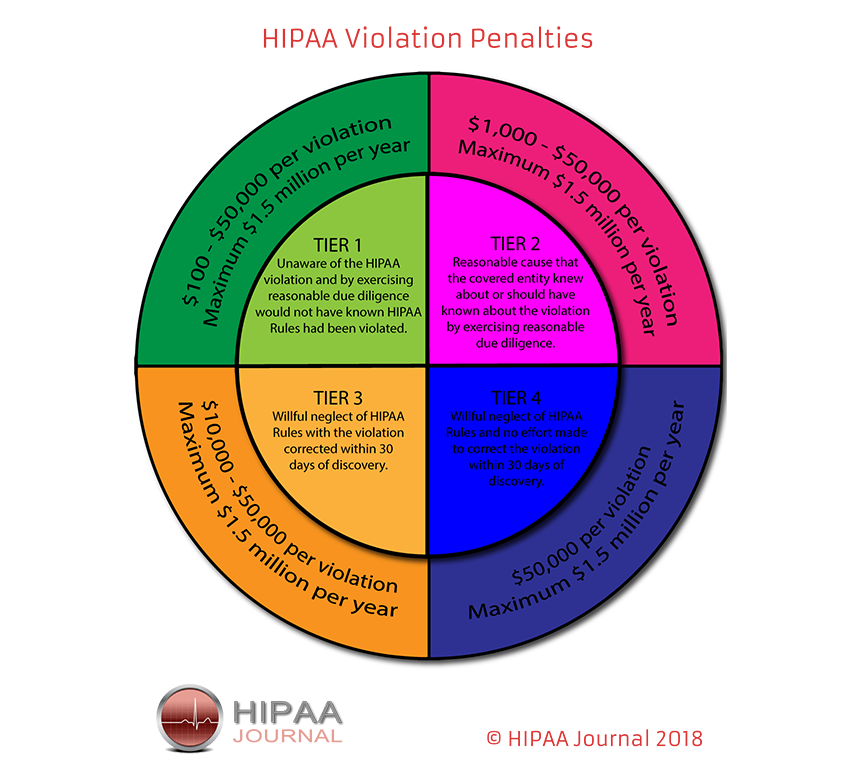
https://www.hipaajournal.com/hipaa-violation-fines/
If you must thank the patient, pick up the phone and call him. Write him a short letter of gratitude. Or thank him in person the next time he visits your office. Thanking someone in-person is always a more memorable experience. It demonstrates you noticed. It’s personal. And it’s devoid of the likely platitude you would have inserted online. It’s hard to come up with original content on a regular basis to express thanks.
Not all patient reviews fit neatly into prescribed categories. How should doctors respond to mixed patient reviews?

Not all reviews are positive. Not all reviews are negative. Some reviews are a mix of positive and negative sentiments – we call them “candid” reviews. A candid review may read something like this…
“The doctor was great. My results are excellent. The lady at the desk always seemed confused though. Would highly recommend!”
Candid reviews are perplexing because they are ambiguous. The example above praised the doctor but was critical of his staff. Will patients perceive this negatively? Positively? Will they care at all? Our answer is: It depends. Pick your battles.
Start by breaking the review apart and assigning character traits to each piece. “The doctor was great” is obviously a positive element. “My results are excellent” may or may not be useful to a new patient. But the statement suggests the author experienced a positive outcome as a result of the physician’s care, so let’s assume that statement is a positive element as well. “The lady at the desk always seemed confused” is a negative element, but unrelated to the quality of care rendered by the attending physician. The final statement “Would highly recommend!” is a positive element.
So – we’re left with three positive elements and one negative element. A positive review, all things considered. We’d suggest leaving this one alone. Remember – every time you respond to a review (positive or negative) you are courting a certain level of risk.
Responding to a patient review is only appropriate when the risk of leaving the review alone exceeds the risk of addressing the review with a carefully constructed response. Crafting a HIPAA compliant response by yourself is possible, and this article’s purpose is to act as a pathfinder. That said, even with proper research, crafting an optimal response can be time-consuming and risky. Professional guidance is indispensable. Many patient reviews are vague. How should doctors respond to negative patient reviews that are short on details?
You won’t always have the luxury of knowing why a patient was dissatisfied with his care. Some reviews will be as brief as: “Bad. Just bad. Trust me, you don’t want to know.” These comments leave little room for the physician to extend an olive branch. What are you going to write? “No, I’m not bad.” Therefore – economize your reply. Your response should achieve the objectives outlined below… Identify why the patient was dissatisfied with his care – once you deduce why the patient is upset, you can attempt to remedy. Present the public with proof the practice is reasonable and willing to discuss perceived wrongdoings. Be firm, but amicable. Negative reviews give physicians an opportunity to defy expectations. The expectation is that you’ll deliver an emotionally-charged reply and validate all the awful things the patient has alleged. Sanitize your reply by stating facts. Doing so will allow you to take back control. Take the conversation offline. No physician has ever profited from indulging in a drawn-out online argument. Present the author with your practice’s phone number. Invite the public to call the practice to discuss their quality of care. 
Sometimes malicious entities (ex-spouses, dismissed employees, angry patients) defame doctors online by posting “fake” patient reviews. What can doctors do to combat fraudulent patient reviews?

A physician’s first instinct is to find some way to remove these fraudulent posts from the web. We do not recommend this strategy. We’ll explain why shortly. Instead, prioritize the collection and publication of fresh patient reviews. Your goal is to dilute the damage caused by the malicious posts by supplanting them with new (hopefully favorable) reviews. Your existing patients will be your lifelines. Be straightforward. Explain to qualified patients (face-to-face) that you value their opinions and are interested in collecting patient feedback. Objective measurements (patient reviews) are the most valuable statistic they can provide.
The next step is to identify where the suspect review is hosted. This is important because it will make it easier for you to direct a patient’s actions. Asking a patient to simply write a review is too broad. Was the fraudulent review posted on Google? If so, encourage patients to post their reviews on Google. Doing so will increase the speed at which the malicious content is displaced.
Competing positive and negative narratives are preferable to only a few negative narratives.
After you identify where the fraudulent post is living, study the website’s Terms of Use. If the review violates this policy, you may be able to successfully petition for the review’s removal. A fair warning, though – this is not a fast process. Review sites are inundated with these requests every day. It will take time before someone puts a pair of eyes on your request. And unless your argument for the review’s removal is ironclad, it likely won’t happen.
Doctors can easily prove to themselves (and their staff) that a review is fake. But doing so achieves nothing. Existing patients do not need to be convinced a review is fake. They are already excellent judges of a physician’s character and skill. Fake reviews are damaging because they have the power to influence the perceptions of new patients – members of the doctor’s community who do not know him well enough to discern fact from fiction. To an outsider like Google, fake patients look identical to real patients.
To prove our point – quickly Google the name of a colleague or a competitor. Examine his patient reviews. If he has received a negative review in the past, study it. Could you, with absolute certainty, prove that the negative review was written by a non-patient? Unless the review references a procedure that you know your colleague does not perform, you can’t know. And neither can Google.
So – what can be done? If you cannot supplant it and you cannot remove it, you must refute it. The incorrect way to go about this is to deliver an emotionally-charged response. You’ll see much better results if you deal only with facts.
Start by studying the review’s content. As we said before – identify opportunities to educate the public. The author’s “real” identity is a “truth” outside of your control. Accusing the author of being a fraud is a waste of time.
Instead, de-escalate the situation by addressing the “truths” you do control – namely the rules and policies your practice abides. Does the review reference a procedure your practice does not offer? Does it reference a staff member who is no longer employed by the practice? Look for holes you can probe. Referencing these inconsistencies in your response will make it clear the testimony is either grossly exaggerated or outright false.
Negative patient reviews trigger arguments between doctors and patients. But what happens when a negative patient review triggers an argument between patients? Do doctors need to play peacemaker?

Doctors are popular people. They work to minimize and relieve the suffering of others. They are not perfect, but people (generally) like them. So, when doctors are criticized online, sometimes members of their community come to their defense. We call these entities “review vigilantes.” These phantom knights will respond to negative reviews and challenge the critic’s assertions. The ensuing arguments often turn ugly. This phenomenon is rare, but it does happen. And while the intentions of these vigilantes are often good, their actions sometimes do more harm than good in the long run.
If this happens to you, contact the vigilante and politely tell him to stop defending you online. You may feel tempted to let the vigilante just “do his thing.” He is, after all, acting in your defense.
We discourage this passive line of thought.
Imagine you’ve been criticized online by a former patient. You respond with strategic intent, but while emotions are still high, another patient joins the conversation. He’s come to your defense. This interference is uninvited. Your vigilante’s response is not strategic. It is likely emotionally charged. It questions your critic’s intelligence, as well as his motivations. This compels the critic to fight back. He assumes you two are in cahoots. The exchange escalates. The argument spreads across your practice’s Google profile. You do not participate. You don’t have to participate – the argument has become self-sustaining. The belligerents feed off one another’s negativity.
The third-parties observing this conflict may arrive at several unfavorable conclusions. They may assume the vigilante is a gopher – an anonymous troll hired by the doctor to police the online space and descend upon perceived malcontent. They may assume the vigilante is a false identity the physician assumes when he wants to engage his critics. Or they may assume the physician simply has limited control of his affairs and is better avoided.
The ultimate objective of any response is to take the conversation offline. Allowing vigilantes to act freely achieves the opposite. If you become a “victim” of this phenomenon, put a stop to it. You’ll inherit any negative consequences brought about by the vigilante’s actions.
With this as backdrop, it is occasionally helpful to have an existing patient weigh in – one and done. No debate, just a single response. It is the back and forth that needs to be avoided.
While thorough, we do not consider this an exhaustive treatise. Additional input from our readers is always welcome. We invite you to share your thoughts in the comments below.
Learn how Medical Justice can protect you from medico-legal mayhem…
Take Advantage of Our Review Monitoring Service
With eMerit, we help you automate review collection and posting to improve your online reputation.
Consult with a Medico-Legal Expert
Medical Justice Founder and CEO, Jeff Segal, MD, JD and our expert team provide consultations to doctors in need of guidance.
Meet the Experts Driving Medical Justice
Our Executive Team walks with our member doctors until their medico-legal obstacles are resolved.
Jeffrey Segal, MD, JD
Chief Executive Officer and Founder
Dr. Jeffrey Segal, Chief Executive Officer and Founder of Medical Justice, is a board-certified neurosurgeon. Dr. Segal is a Fellow of the American College of Surgeons; the American College of Legal Medicine; and the American Association of Neurological Surgeons. He is also a member of the North American Spine Society. In the process of conceiving, funding, developing, and growing Medical Justice, Dr. Segal has established himself as one of the country’s leading authorities on medical malpractice issues, counterclaims, and internet-based assaults on reputation.
Dr. Segal was a practicing neurosurgeon for approximately ten years, during which time he also played an active role as a participant on various state-sanctioned medical review panels designed to decrease the incidence of meritless medical malpractice cases.
Dr. Segal holds a M.D. from Baylor College of Medicine, where he also completed a neurosurgical residency. Dr. Segal served as a Spinal Surgery Fellow at The University of South Florida Medical School. He is a member of Phi Beta Kappa as well as the AOA Medical Honor Society. Dr. Segal received his B.A. from the University of Texas and graduated with a J.D. from Concord Law School with highest honors.
In 2000, he co-founded and served as CEO of DarPharma, Inc, a biotechnology company in Chapel Hill, NC, focused on the discovery and development of first-of-class pharmaceuticals for neuropsychiatric disorders.
Dr. Segal is also a partner at Byrd Adatto, a national business and health care law firm. With decades of combined experience in serving doctors, dentists, and other providers, Byrd Adatto has a national pedigree to address most legal issues that arise in the business and practice of medicine.




As always, solid advice. I am the practice and laboratory manager, and one type of negative review has irked me in particular. One patient decided to name one of the nurses by first name AND designate where she sits in order to belittle her publicly and opine that she was rude and unprofessional. Having witnessed the event at hand, I know that she was neither, but she was firm and kind with her words. I asked Google if they could remove her first name and they said they would not. This seems like a bit of an attack on an employee’s safety. As a manager, I feel somewhat responsible for mitigating risks of my staff being attacked. Is Google correct? As a general rule, we do NOT respond online to reviews, positive or negative.